- Archived Webinar: Misophonia: What is known, what is unknown, and where we go from here – aired on Wednesday, Jan. 15, 2025 at 1PM ET
 DATE: Wednesday, January 15, 2025 at 1PM ET
DATE: Wednesday, January 15, 2025 at 1PM ET
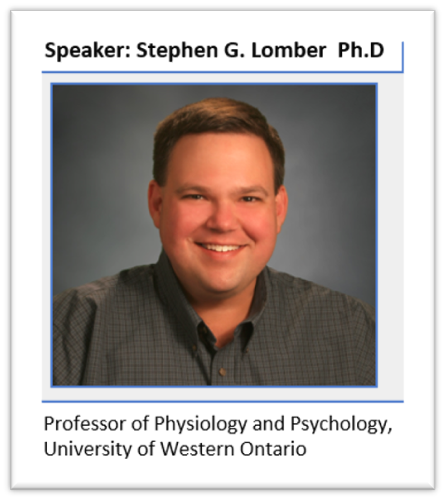
SPEAKER: Blake Butler, Blake Butler, Assistant Professor of Psychology, UWO, Investigator, National Centre for Audiology
Abstract:
Misophonia is a disorder of decreased tolerance to specific sounds or stimuli associated with such sounds. These stimuli, known as “triggers,” are experienced as unpleasant or distressing and tend to evoke strong negative emotional, physiological, and behavioral responses that are not seen in most other people. While estimates suggest 5% or more of the general population may experience misophonia, little is known about the specific patterns of deficits underlying these symptoms; as a result, misophonia is not currently included in diagnostic manuals like the DSM-V. Because misophonia lies at the interface of sound intolerance and psychopathology, individuals experiencing this disorder are likely to present to an audiologist at a first point of clinical contact should they seek treatment. Accordingly, it is critical that clinicians be prepared with enough background knowledge to engage in meaningful discussion and treatment planning.
In this webinar, I will attempt to provide an overview of the (brief) history of misophonia, including the recent development of a consensus definition and evolving evidence that misophonia represents a standalone disorder that cannot be explained by symptoms associated with other sound tolerance disorders (e.g., hyperacusis) or psychopathologies (e.g., generalized anxiety, obsessive-compulsive disorder). I’ll discuss the various ways in which the experience of misophonia can negatively impact an individual’s daily life, and the ways in which they may act to compensate for their symptoms. Finally, I will summarize empirical evidence by our group and others outlining potential deficits in mechanisms associated with distractor suppression that may underlie the disorder. The overall goal of the discussion is to provide insights into the development and experience of misophonia that will inform positive clinical interactions with individuals presenting with these symptoms.
Learning Objectives
- Misophonia is a standalone sound tolerance disorder
- ‘Trigger sounds’ evoke atypical physiological and psychological responses
- Misunderstanding and misdiagnosis have impacted the development of meaningful interventions
SPEAKER BIO: Blake Butler, Blake Butler, Assistant Professor of Psychology, UWO, Investigator, National Centre for Audiology
Dr. Blake Butler is an assistant professor in the Department of Psychology and the Centre for Brain and Mind, and an investigator at the National Centre for Audiology at the University of Western Ontario. Dr. Butler and his research team are interested in the role of experience & plasticity in the typical and atypical development of sensory systems, with a focus on hearing loss and restoration. Their program combines behavioural, neuroimaging, and histological approaches in humans and animal models to examine how the structure and function of sensory cortices are shaped by early development.
- Archived Webinar: Successful Pathways to Outcomes in Bilateral Cochlear Implantation Aired on Wednesday, March 19, 2025 at 1PM
 DATE: Wednesday, March 19, 2025 at 1PM ET
DATE: Wednesday, March 19, 2025 at 1PM ET
SPEAKER: Ruth Litovsky, PhD, Oros Bascom Chair & Professor, Waisman Centre, Department of Communication Sciences & Disorders, University of Wisconsin
Abstract:
Binaural hearing is a critically important auditory process which enhances our ability to navigate in noisy, complex listening environments. Bilateral cochlear implants are provided to a growing number of children, and adults, depending on the standard of care and insurance coverage. Bilateral hearing typically improves localization of sounds and segregation of speech from background noise compared with unilateral hearing. However, patients typically perform worse than normal hearing listeners. We use several approaches to understand factors that contribute to reduced performance in individuals with BiCIs. One factor is the asymmetry in hearing across the ears, which reduces how well information across the two ears is integrated, fused, and leads to good spatial hearing. A second factor is difference across the ears in neural health; poor neural health can include many aspects of reduced ability of the neural element to encode and transmit information with fidelity. In the binaural system, poor neural health in one of the two ears can promote a ‘bottleneck’ for information processing, meaning that even if one ear transmits good information, lack of fidelity in the other ear promotes poor binaural hearing. Because CI processors do not preserve binaural cues with fidelity, we use research processors to generate multi-channel binaural stimulation strategies that introduce different rates of stimulation across the electrode arrays, thereby preserving rates that are important for both binaural sensitivity and speech understanding. In addition, eye gaze studies reveal developmental factors that in decision-making that are not observed with measures of threshold. Finally, pupillometry studies provide insight into the impact of integrating inputs from two ears, whereby in some instances improved performance with two ears can be “costly” in the listening effort domain.
Learning Objectives
- Understand binaural hearing processes in individuals with normal hearing, and limitations in individuals with hearing loss.
- Understand current outcomes in individuals with bilateral cochlear implants and limitations that need to be addressed.
- Understand future directions in improving outcomes in bilateral cochlear implants, including segregation of speech in noise, sound localization and reduction in listening effort.
SPEAKER: Ruth Litovsky, PhD, Oros Bascom Chair & Professor, Waisman Centre, Department of Communication Sciences & Disorders, University of Wisconsin
Ruth Litovsky, PhD, is Oros Family chair in the Department of Communicative Sciences and Disorders at the University of Wisconsin – Madison. She has a joint appointment in the Division of Otolaryngology in the Department of Surgery, and serves as the Academic Associate Dean for the Division of Natural, Physical & Mathematical Sciences in the College of Letters & Science.
Ruth received her BA and MA degrees from Washington University in St. Louis (1987), PhD in Developmental Psychology under the mentorship of Rachel Clifton (Keen) in from the University of Massachusetts-Amherst (1991), and then forged into the world of auditory neuroscience where she trained with Tom Yin as a postdoctoral fellow at the University of Wisconsin-Madison (1991-1994). She spent the next seven years combining studies in human behavior and auditory neuroscience, at Boston University in Steve Colburn’s lab, and at the Massachusetts Eye and Ear Infirmary.
Scientifically, Ruth’s work has revealed fundamental insights into the perceptual capabilities of binaural and spatial hearing in human listeners. During much of her career, she studied sound localization, binaural hearing, source separation, speech intelligibility, echo suppression and how experience and impacts perception and auditory development. Since joining the faculty at the University of Wisconsin-Madison (2001), her research has focused primarily on auditory function in children and adults with bilateral cochlear implants, with an eye towards ultimately improving outcomes in cochlear implant users. In recent years, Ruth has also embarked on studies in individuals with single-sided deafness, and a very new area of research on individuals with Down Syndrome to understanding hearing loss, cognition, language and brain structure. Ruth’s lab is unique in that the approaches that are used to delve into novel scientific inquiry are ever evolving. While they include psychophysics and reverse engineering to explore how binaural hearing can be restored cochlear implant users with fidelity, pupillometry and eye gaze measures are harnessed to examine ‘real time’ processing of information and listening effort during perceptual tasks. More recently, the lab has begun to implement functional neuroimaging to investigate neural signatures for bilateral benefits and cognitive load.
Ruth is passionate about mentoring and service to her community. She has served on numerous committees and panels at her home institution and in service to scientific organizations. She believes that the only way to conduct research through the mentorship of students and postdocs, as well as through collaboration with colleagues around the world. She attributes the outcomes of her research program, the success of the lab and impact of the work to her scientific family and the many long-lasting relationships forged through teaching, mentoring and collaboration. The energy and passion that Ruth puts into her science is matched by her commitment to diversity, equity, inclusion and belonging, as well as mentorship. She has devoted much of her career to developing mentoring programs at scientific conferences and organizations and has helped organizations adopt best practices to address systemic problems.
Ruth’s recognition for her scientific achievements can be seen in her sustained record of research excellence. Her ongoing research program has been continuously funded by grants from NIH-NIDCD since 1995, in addition to grants from smaller foundations and collaborative projects with cochlear implant companies. She has published over 150 papers and book chapters based on her research which focuses hearing abilities covering lifespan of humans to include infants and elderly adults.
Ruth has received several awards during her career. She was the first woman to receive the Silver Medal from the Acoustical Society of America. She was honored with Carhart Memorial Lecture of the American Auditory Society, was a Fulbright Senior Fellow, Elected Fellow of the Acoustical Society of America, was President the Association for Research in Otolaryngology, elected chair of the Auditory System Gordon Research Conference, invited to give the 2024 American Cochlear Implant Alliance Keynote honoring the life and career of Dr. John Niparko. and is now the Editor in Chief of the journal Ear and Hearing.
- Archived Webinar: Opportunities and challenges for assistive listening with Bluetooth LE Audio and Auracast aired Wednesday, Oct 16, 2024 at 1PM ET
 DATE: Wednesday, October 16, 2024 – 1 PM ET
DATE: Wednesday, October 16, 2024 – 1 PM ET
SPEAKER: Ian C. Bruce, Ph.D., P.Eng., Professor of Electrical & Computer Engineering, McMaster University, Hamilton, Ontario
Abstract:
Over the past decade, the hearing aid industry has been working with the Bluetooth organization to develop a new Bluetooth audio standard that is capable of low-energy, low-delay, high-fidelity audio streaming and broadcasting. This standard was finalized in September 2020, with the names Bluetooth® LE Audio and Auracast™, and hearing aid and consumer audio products that support this standard are now starting to come on the market. Bluetooth LE Audio and Auracast are now poised to supersede the interim Apple Made for iPhone (MFi) and Android Audio Streaming for Hearing Aids (ASHA) protocols, propriety TV audio streamers available from hearing aid manufacturers, and eventually telecoil hearing loop systems.
This webinar will provide an overview of what new capabilities are available via this new Bluetooth standard and what opportunities it presents for improved assistive listening experiences in a variety of scenarios. The presentation will also discuss a number of remaining challenges faced by hearing aid and audio equipment manufacturers, assistive listening system installers and audio system operators, and hearing aid users and audiologists, that will need to be overcome in order to provide an optimal listening experience for all users of the technology.
Learning Points:
- What are Bluetooth LE Audio and Auracast, and how do they differ from previous versions of Bluetooth?
- How can Auracast be used in different assistive listening scenarios, and what are the remaining challenges in developing standards and best practices for Auracast usage?
- How will audiologists be able to advise and support their clients in obtaining the maximum benefit from Bluetooth LE Audio and Auracast?
SPEAKER BIO: Ian C. Bruce, Ph.D., P.Eng., Professor of Electrical & Computer Engineering, McMaster University, Hamilton, Ontario
Ian Bruce completed his Bachelor’s degree in Electrical and Electronic Engineering at the University of Melbourne, Australia, in 1993 and then worked for a year as a Research and Teaching Assistant at the University of Technology in Vienna, Austria. He was subsequently a PhD student at the Bionic Ear Institute in Melbourne, receiving his doctorate from the University of Melbourne in 1998. From 1998 to 2001, Ian did a Postdoctoral Fellowship in the Department of Biomedical Engineering at the Johns Hopkins University in Baltimore, Maryland, USA.
In 2002, Ian joined the faculty at McMaster University, Hamilton, Canada. He is currently a Professor in Electrical & Computer Engineering at McMaster, as well as being engaged in interdisciplinary research and academic activities in hearing sciences, biomedical engineering, neuroscience, psychology, and music cognition. His research is focused on applying cutting-edge experimental and computational methods to better understand, diagnosis and treat hearing disorders.
- Archived Webinar: Strategic Practice Management Planning for Audiology Private Practice aired on Wednesday, Nov. 20, 2024 at 1PM ET
 DATE: Wednesday, November 20, 2024 – 1 PM ET
DATE: Wednesday, November 20, 2024 – 1 PM ET
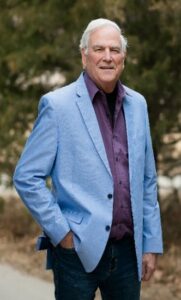
SPEAKER: Robert M. Traynor, Ed.D., MBA, FNAP, ABAC, CCC-A, Adjunct Professor of Audiology, Salus University
Abstract:
After some years of clinical experience, audiologists often become disenchanted with the corporate manipulation of their career and look forward to owning their own practice. As practitioners move into the private sector owning their own audiology business, they need to understand fundamental business principles. Entrepreneurship, general economics, business planning, sales techniques, competitive strategies, human resources, marketing, and other essential basics for the development and maintenance of a business operation.
While limited in its timeframe, the webinar will review the essential business considerations audiology clinic management.
Learning Objectives
Upon completion, participants will be able to
- Describe the characteristics of an entrepreneur within the field of Audiology.
- Describe the pre and formal process of preparing a written business plan.
- Describe the unexpected business skills required for practice owners to ensure success.
SPEAKER BIO: Robert M. Traynor, Ed.D., MBA, FNAP, ABAC, CCC-A, Adjunct Professor of Audiology, Salus University
Dr. Robert M. Traynor practiced audiology 46 years at Audiology Associates, Inc., Greeley, Colorado, USA, providing diagnostic & rehabilitative treatment for hearing loss/tinnitus patients of all ages & operative monitoring for otolaryngologists & general surgeons. He holds degrees: University of Northern Colorado (BA, 1972; MA, 1973; EdD, 1975), University of Phoenix (MBA, 2006), conducted Audiology postdoctoral study at Northwestern University (1984). He served in the U.S. Air force and 16 years in U.S. Army Reserve as a military audiologist retiring Lt. Colonel in 1998.
1972-1993, Dr. Traynor was Instructor, Assistant Professor, Associate Professor of Audiology, University of Northern Colorado, Professor & Audiology Program Director, Colorado State University. 1999-2020, Audiology Adjunct faculty at the University of Florida teaching Counseling and Audiology Practice Management. He currently is Adjunct Professor at University of Arkansas/Medical Sciences, Rush University, and Salus University.
In 2019, Dr. Traynor was awarded the Joel Wernick Award from the Academy of Doctors of Audiology, 2018 became a Distinguished Alumnus: University of Northern Colorado, in 2017 was inducted as Fellow of the National Academies of Practice and is the recipient of the 2014 Colorado Academy of Audiology Lifetime Achievement Award.
Dr. Traynor and his coauthor, Dr. Brian Taylor, recently submitted the manuscript for Strategic Practice Management, 4th Edition, which currently is “in press”, and will be available March 2025.
At Robert Traynor Audiology, LLC, he provides professional advice & consulting to the hearing industry and Forensic Audiology services.
- Archived Webinar: Audiological considerations and speech perception outcomes for children and adults living with Down syndrome – Aired Wednesday, Sept 18, 2024 at 1PM ET
 DATE: Wednesday, September 18, 2024 – 1 PM ET
DATE: Wednesday, September 18, 2024 – 1 PM ET
SPEAKER: Lori Leibold, Ph.D. Director, Center for Hearing Research, Boys Town National Research Hospital
Abstract:
Rates of conductive, sensorineural, and mixed hearing loss are higher for individuals living with Down syndrome relative to individuals who are neurotypical. However, individuals living with Down syndrome have been underrepresented in hearing research studies, which has in turn contributed to hearing health care disparities such as reduced use of amplification.
This webinar will provide an overview of scientists at Boys Town National Research Hospital to characterize how speech, language, and hearing develop across the lifespan for individuals living with Down syndrome. Results from studies designed to characterize the audiological profile of school-age children and adults living with Down syndrome will be discussed, including age-related changes in conventional and extended high-frequency audiometric thresholds. Speech perception data in competing noise and in competing speech will be presented, considering the influence of listener factors such as age, language skills, executive function, and audibility. Finally, considerations for working with individuals living with Down syndrome and their families will be discussed.
Key learning points
Upon completion of this session, the participant will be able to:
- Describe the unique hearing and speech perception challenges faced by individuals living with Down syndrome across the lifespan.
- Discuss considerations for audiological assessment of individuals living with Down syndrome.
- Consider barriers that limit communication outcomes for individuals living with Down syndrome.
SPEAKER BIO: Lori Leibold, Ph.D. Director, Center for Hearing Research, Boys Town National Research Hospital
Lori Leibold is the Director of the Center for Hearing Research and leads the Human Auditory Development Laboratory at Boys Town National Research Hospital in Omaha, Nebraska. She reviewed her B.S. from McMaster University, M.Sc. in Audiology from the University of Western Ontario, and her Ph.D. from the University of Washington. Her background is in audiology and developmental psychoacoustics. Her research is focused on understanding how and when hearing and speech perception develop across infancy and childhood, which includes studies evaluating the speech perception and auditory abilities of infants, children, and adults living with Down syndrome. Working with a team of scientists, clinicians, and community engagement specialists, she is involved in multiple efforts to increase participation rates, promote programmatic longevity, and improve hearing health outcomes for individuals living with Down syndrome. These efforts include coordination of a community advisory board and travel to rural and/or underserved communities to conduct research in our mobile research vehicle.
- Archived Webinar: Update on Infant Hearing Health Services in Canada: 2024 Report Card aired on Wednesday, Nov. 13, 2024 at 1PM ET
 DATE: Wednesday, November 13, 2024 – 1 PM ET
DATE: Wednesday, November 13, 2024 – 1 PM ET
SPEAKER: Marlene Bagatto (on behalf of the Canadian Infant Hearing Task Force), Assistant Professor School of Communication Sciences and Disorders, National Centre for Audiology, Western University
Abstract:
Early hearing detection and intervention (EHDI) programs are available worldwide to proactively address hearing health in infants and children. Along with universal hearing screening of newborns, a comprehensive and effective EHDI program also includes a complete hearing assessment to confirm the presence or absence of permanent hearing loss, intervention services including technology and language development, family support as well as monitoring and evaluation of the program using a database. Without all five components, access to timely and high-quality hearing health services for infants cannot be achieved. During this presentation, the results of the Canadian Infant Hearing Task Force’s most recent Report Card describing the status of EHDI programs across Canada will be shared. Data were gathered through a country-wide survey which will be described. Results from this work revealed that, although there has been some improvement in certain provinces and territories, Canada continues to remain insufficient in offering comprehensive, accessible, and sustainable EHDI programs. Continued action from Canada’s governments in addition to federal policy leadership is needed to achieve sufficient and sustainable EHDI programs.
Learning Objectives
Participants to this presentation will be able to:
- Describe the components of a comprehensive EHDI program.
- Explain the status of EHDI programs across Canada.
- Discuss actions to improve access to infant hearing health services in provinces/territories.
SPEAKER BIO: Marlene Bagatto (on behalf of the Canadian Infant Hearing Task Force), Assistant Professor School of Communication Sciences and Disorders, National Centre for Audiology, Western University
Marlene Bagatto is an Assistant Professor in the School of Communication Sciences and Disorders and the National Centre for Audiology at Western University in London, Ontario, Canada. The research in her Pediatric Audiology Strategies and Systems Laboratory focusses on policy and practice integration for infant and child hearing. Dr. Bagatto is a consultant for early hearing detection and intervention (EHDI) programs in several Canadian provinces to develop and implement protocols for various components of infant hearing health care. Dr. Bagatto is Past President of the Canadian Academy of Audiology, Past Chair of the Canadian Infant Hearing Task Force, and the 2023 recipient of the Marion Downs Award in Pediatric Audiology from the American Academy of Audiology.
- Archived Webinar: Tools to help determine when patients should be referred for a cochlear implant candidacy evaluation with Terry Zwolan – Aired March 20, 2024 at 1pm ET
 DATE: Wednesday, March 20, 2024 – 1 PM ET
DATE: Wednesday, March 20, 2024 – 1 PM ET
SPEAKER: Terry Zwolan, Ph.D., CCC-A, Director, Audiology Access and Standard of Care – Cochlear Americas and Professor Emerita, Michigan Medicine, Department of Otolaryngology – Head and Neck Surgery
Abstract:
The value of cochlear implants (CIs) as a treatment for significant hearing loss has been well demonstrated. However, current estimates indicate that only about 5-10% of adult cochlear implant candidates who could benefit from a CI actually receive one. This low adoption of treatment may be due, at least in part, to recent changes in CI candidacy and uncertainty of audiologists regarding when a patient should be referred for a cochlear implant candidacy evaluation (CICE). It is valuable for all audiologists to understand when patients should be considered for alternative hearing technology.
This presentation will provide information regarding the 60/60 Guideline, which simplifies referral decisions by providing guidance based on routine audiologic evaluations. Procedures used to develop the 60/60 will be described, and recent reviews of it’s clinical utility will be discussed. Additional measures to aid in referral decisions will also be described. The presentation will include a list of possible reasons some patients hesitate to move forward with a CICE. Counseling tools that can be used by clinicians to educate patients about CICEs will be discussed, including a description of the procedures patients participate in as part of CI Candidacy evaluations.
Learning Objectives:
- Explain the 60/ 60 referral guideline and how it can be used to identify patients who should be referred for a cochlear implant candidacy evaluation (CICE)
- Describe, for patients, procedures that are typically included in a CICE
- Answer questions that patients often have about attending a CICE
SPEAKER BIO: Terry Zwolan, Ph.D., CCC-A, Director, Audiology Access and Standard of Care – Cochlear Americas and Professor Emerita, Michigan Medicine, Department of Otolaryngology – Head and Neck Surgery
Terry Zwolan joined Cochlear Americas in November 2022 as the Director of Audiology Access and Standard of Care. In her role, she oversees two Cochlear Hearing Centers in Texas and works on various initiatives to improve access to care. Prior to joining Cochlear, she was Director of the Cochlear Implant Program at the University of Michigan from 1990-2021 and is Professor Emerita in the Department of Otolaryngology – Head and Neck Surgery. She previously served as Course Director for the Institute for Cochlear Implant Training (ICIT), served as an adjunct professor for Wayne State University’s AuD program, and is a co-founder and past member of the Board of Directors of the American Cochlear Implant (ACI) Alliance. She is currently leading efforts to roll out Version 3 of the Minimum Speech Test Battery for evaluating CI candidacy in the United States.
CAA is grateful to Cochlear Canada for sponsoring this speaker

- Archived Webinar: Music and Hearing Aids with Marshall Chasin – Aired April 17, 2024 at 1pm ET
 DATE: Wednesday, April 17, 2024 – 1 PM ET
DATE: Wednesday, April 17, 2024 – 1 PM ET
SPEAKER: Marshall Chasin, Au.D., reg. CASLPO, Marshall Chasin and Associates
Abstract:
Music and speech have some differences which include spectral shape, intensity and “crest factors”. Most modern digital hearing aids cannot handle the more intense inputs that are characteristic of music. Four new technologies and four clinical strategies will be provided to optimize hearing aids for music as well as for speech. These technologies are designed to circumvent some problems associated with the analog-to-digital conversion process- a major weak point with many modern hearing aids. Audio files will be showing the problems of the hearing aid not being able to handle the higher level signals associated with music, as well as demonstrating the difficulties with frequency compression for music.
Learning Objectives:
After attending this seminar, the participant should be able to:
- Select software programming that is optimized for music
- Explain the engineering limitations of most modern hearing aids for music
- Identify some simple clinical strategies to improve a hearing aid for music
SPEAKER BIO: Marshall Chasin, Au.D., reg. CASLPO, Marshall Chasin and Associates
Dr. Marshall Chasin is Head of Audiology at the Musicians’ Clinics of Canada, Adjunct Professor at the University of Toronto (in Linguistics), and Adjunct Professor at Western University. Marshall holds a B.Sc. in Mathematics and Linguistics from the University of Toronto, a M.Sc. in Audiology and Speech Sciences from the University of British Columbia and his AuD from the Arizona School of Health Sciences. He is the author of over 200 articles and 8 books including Music and Hearing Aids (Plural Publishing, 2022). Marshall writes a monthly column in Hearing Review called Back to Basics, and has been the recipient of many awards over the years including the 2004 Audiology Foundation of America Professional Leadership Award, the 2012 Queen Elizabeth II Silver Jubilee Award, the 2013 Jos Millar Shield award from the British Society of Audiology and the 2017 Canada 150 Medal. He has developed a TTS app called Temporary Hearing Loss Test app.
- Archived Webinar: Development of Inner Ear Medicines for Threshold and Supra-threshold Indications with Colleen Le Prell – Aired May 24, 2023 at 1pm ET
DATE: Wednesday, May 24, 2023 – 1 PM ET
SPEAKER: Colleen Le Prell, Emilie and Phil Schepps Professor of Hearing Science Head, Department of Speech, Language, and Hearing The University of Texas at Dallas
Abstract:
The phrase “hidden hearing loss” has been used to refer to 1) decreased amplitude of wave I of the auditory brainstem response (ABR) in the absence of threshold deficits; 2) loss of the synaptic connections between the inner hair cells (IHCs) and the auditory nerve dendrites (“cochlear synaptopathy”) in the absence of outer hair cell (OHC) loss; and 3) tinnitus, hyperacusis, hearing-in-noise deficits, or other suprathreshold hearing disorders that occur independent of hearing loss. The anatomical pathology and supra-threshold functional deficits have been termed “hidden” because they are not captured by the measures most commonly used during human audiometric assessment (the audiogram, and otoacoustic emission (OAE) tests) or in animal studies (ABR threshold, OAE threshold or amplitude, OHC counts). In reality, hearing-in-noise difficulties and tinnitus are common patient complaints, not-so-hidden to either the patient or the audiologist when the appropriate test battery is completed. With increasing recognition of the importance of these supra-threshold complaints has come interest in the potential for treatment using medicines that protect or repair the inner ear sensory cells.
This session will briefly review specific patterns of cell death, changes in sound evoked OAE and ABR responses, and both threshold shift and deficits “beyond the audiogram” that can be measured in clinical and research laboratory settings. The inclusion of threshold and supra-threshold tests within the current clinical trial landscape will be reviewed and considerations in the design of clinical trials will be discussed. At this time, there are no drugs approved by the FDA for “hidden hearing loss” indications, but there is an active drug development pipeline with major efforts across academic labs, pharmaceutical and biotechnology companies, and venture capital investments.
Learning Points:
After this presentation, participants will be able to:
- Describe suprathreshold deficits that are commonly captured under the umbrella of hidden hearing loss
- Identify diagnostic test batteries relevant for documentation of suprathreshold deficits
- Summarize the current status of drug development for suprathreshold hearing deficits
SPEAKER BIO: Colleen Le Prell, Emilie and Phil Schepps Professor of Hearing Science Head, Department of Speech, Language, and Hearing The University of Texas at Dallas
Colleen Le Prell, Ph.D., is the Emilie and Phil Schepps Professor of Hearing Science, Chair of the Department of Speech, Language, and Hearing, and Program Head for the Ph.D. Program in Speech, Language, and Hearing Sciences at the University of Texas at Dallas. Dr. Le Prell has received research funding from government, industry, and philanthropic sources for clinical, translational, and applied research in her laboratory. Programmatic research in her laboratory advances the understanding and prevention of noise-induced hearing loss. She is currently mentoring three AuD-PhD students and six AuD students on NIHL-related research projects and interests. Dr. Le Prell has published 79 peer-reviewed articles and 21 book chapters, and she has edited or co-edited five journal special issues and three books on topics related to her research interests.
In addition to her teaching and research responsibilities, Dr. Le Prell is highly engaged in professional service related to hearing loss prevention and scientific review. She previously served as President for the National Hearing Conservation Association (NHCA), is currently a member of the CDC-NIOSH National Occupational Research Agenda (NORA) Hearing Loss Prevention Cross Sector Council, and she is an invited participant in annual consultations of the World Health Organization – International Telecommunication Union (WHO-ITU) “Make Listening Safe” campaign. She serves as an Associate Editor for the Journal of the Acoustical Society of America and the International Journal of Audiology and she serves on the editorial board for Hearing Research. She is a member of the Auditory System (AUD) Study Section for National Institutes of Health Center for Scientific Review.
- Archived Webinar: Auditory Wellness: What is it? Why is it important? How can it be self-managed? What is the role of audiologists with Larry E. Humes – aired May 15, 2024 at 1pm ET
 DATE: Wednesday, May 15, 2024 – 1 PM ET
DATE: Wednesday, May 15, 2024 – 1 PM ET
SPEAKER: Larry E. Humes, Ph.D., Distinguished Professor Emeritus, Department of Speech, Language, and Hearing Sciences, Indiana University
Abstract:
In this presentation, the concept of auditory wellness will be described, including its connections to other wellness domains and overall well-being. It will be shown that millions of U.S. adults have reduced auditory wellness and have not been served well by the prevailing professional-driven hearing healthcare model. For many with reduced auditory wellness, hearing aids and communication training represent the interventions with the greatest likelihood of improving auditory wellness. Yet, for the many adults with reduced auditory wellness, only about 15-20% have obtained hearing aids through the prevailing hearing healthcare system. For the first time since the development of the modern-day electronic hearing aid over 75 years ago, persons with reduced auditory wellness have been empowered to manage and improve their auditory wellness through self-fitting of over-the-counter (OTC) hearing aids. The self-fitting of hearing aids has been found to be efficacious and effective using several approaches. The fitting of the device, however, is just an initial step, albeit an important one, toward the restoration of optimal auditory wellness. For OTC hearing aids to have the desired impact on those with reduced auditory wellness, many additional self-driven aids and tools must be developed. Viable tools already exist and just need to be made broadly available to those seeking help through OTC hearing aids. In many cases, these tools can be used in collaboration with audiologists to guide the adult with less-than-optimal auditory wellness through their journey to improved auditory wellness. Some of these tools and approaches to their use will be described here. The goal is the creation of a self-empowered, self-driven pathway to improved auditory wellness for adults, an outcome that can be facilitated through collaborations with audiologists.
Learning Objectives:
- “Auditory wellness” is critical to achieving a thriving well-being and overall satisfaction with life, yet millions of adults have reduced auditory wellness.
- “Auditory wellness” is not the same as “hearing wellness”, the latter tied exclusively to the pure-tone audiogram and only capturing the bodily-impairment component of healthy function.
- Over-the-Counter (OTC) hearing aids represent only one component of the process of improving auditory wellness. Training in communication strategies, in addition to or instead of the acquisition of devices, is as critical as the selection and fitting of the devices, yet few self-driven, easily accessible tools have been developed to meet the individual’s needs to date.
SPEAKER BIO: Larry E. Humes, Ph.D., Distinguished Professor Emeritus, Department of Speech, Language, and Hearing Sciences, Indiana University
Larry E. Humes earned his undergraduate degree from Purdue University and a master’s degree from Central Michigan University, before completing his Ph.D. at Northwestern University. He then spent 8 years on the faculty at Vanderbilt University before joining the faculty at Indiana University, where he remains today as Distinguished Professor Emeritus. He has published over 175 articles in peer-reviewed journals and another 60 non-peer-reviewed articles, reviews, chapters, and books. He has presented or been a co-presenter on over 380 presentations throughout the world.
Professor Humes has received the Honors of the Association and the Kawana Award for Lifetime Achievement in Publications from the American Speech-Language-Hearing Association, the Jerger Career Award for Research in Audiology from the American Academy of Audiology and presented the 2020 Carhart Memorial Lecture at the annual meeting of the American Auditory Society. He is a Fellow of the Acoustical Society of America and the International Collegium of Rehabilitative Audiology (ICRA).
- Archived Webinar: Cochlear Implantation and Single-Sided Deafness with Kari Smilsky – Aired May 26, 2022 at 2pm ET
Date: Thursday, May 26th – 2pm EST
SPEAKER: Kari Smilsky, Senior Audiologist, Cochlear Implant Program, Sunnybrook Health Sciences Centre Lecturer, University of Toronto: Otolaryngology – Head and Neck Surgery
, CAA Members View the Recording - log in to view
Abstract:
Single sided hearing loss poses significant challenges to communication despite having one normal hearing ear. Individuals with single sided deafness (SSD) report decreased hearing in the presence of background noise and poor localization ability. Traditional treatments for SSD involve contralateral routing of sound via a conventional acoustic CROS hearing aid or via bone conduction. These treatment modalities offer little in the way of improving localization or squelch. Candidacy criteria for cochlear implants (CI) have expanded considerably over the past thirty years and patients with SSD are now an emerging population of candidates for cochlear implantation.
In this webinar, we will review the evolution of cochlear implant candidacy from bilateral profound hearing loss to considering single-sided deafness. The challenges in evaluating objective and subjective outcomes of a cochlear implant in the context of a normal hearing ear will be summarized along with a discussion of a variety of ways to quantify benefit. Results will be presented from a study group of more than seventy recipients who have received a cochlear implant for single-sided deafness. The importance of auditory rehabilitation will be summarized along with factors that may influence outcomes.
Learning Points:
1. What are the binaural benefits of providing a cochlear implant for single-sided deafness?
2. What factors should be considered to determine candidacy for a cochlear implant for single-sided deafness?
3. How can subjective questionnaires complement objective measures to quantify outcomes of a cochlear implant for single-sided deafness?
SPEAKER BIO: Kari Smilsky, Senior Audiologist, Cochlear Implant Program, Sunnybrook Health Sciences Centre Lecturer, University of Toronto: Otolaryngology – Head and Neck Surgery
Kari Smilsky is an audiologist who has been employed at Sunnybrook Health Sciences Centre in Toronto for the past twenty-two years. She has worked with the Cochlear Implant Program since 2006. Kari holds a Masters of Clinical Science Degree from the University of Western Ontario in Communication Disorders and a Bachelor of Science Degree from McMaster University. In additional to working clinically with cochlear implant patients, Kari’s research interests include bilateral cochlear implants, single-sided deafness, auditory brainstem implants, hearing preservation, and the expansion of cochlear implant candidacy. Through her involvement in the Canadian Cochlear Implant Centres Group, Kari has been involved in the development of national clinical standards for bilateral cochlear implant candidacy and provision of cochlear implants for single-sided deafness. Kari sits on the Audiology Advisory Board
, CAA Members View the Recording - log in to view
- Archived Webinar: IDA Webinar – Improving Client Motivation and Satisfaction Through Person-Centered Care With Ena Nielsen & Helle Gjønnes Møller – Aired February 24, 2022
Aired: Thursday February 24 – 12 PM ET
SPEAKER: Ena Nielsen, Associate Director & Helle Gjønnes Møller, Communications Specialist and Project Manager at the Ida Institute
HOST: Sarah Mason, CAA Director and Past CAA President, Dalhousie University
FREE for all – Click to Watch Now
Abstract:
Research shows that supporting clients to be actively involved in their own care not only improves their motivation to go ahead with care – it also helps create better treatment outcomes and increases client satisfaction. This approach of actively involving clients in their own treatment is often referred to as person-centered care (PCC).
Over the past decade, the acknowledgement of PCC has been steadily growing and it is increasingly being integrated in standards and regulations globally, such as ISO 21388, the first international standard for hearing aid fitting management. However, the process of introducing and delivering PCC is still slow in places – and many hearing care professionals feel they would benefit from more dedicated training in the area.
This webinar outlines the fundamental principles of PCC and breaks down the concept into distinct and manageable parts. What, for example, does it mean to show empathy, listen actively, and to involve clients in shared decision-making and goal-setting? And how can you involve family members in a meaningful and productive way? To inspire further learning and exploration of PCC, participants will also be introduced to Inspired by Ida – a program established to help hearing care professionals implement PCC in their everyday practice. Finally, Inspired by Ida members, Kimberly A. Eskritt from Lambton Audiology Associates and Karine Bossé from Echo Audiology, will share some concrete examples of how PCC makes a difference in their clinical practice.
Learning Points:
After watching this webinar, participants will be able to
-
- Describe what PCC is and what the benefits are for clients and HCPs
- Begin to apply the principles of PCC in daily practice
- Understand how the Inspired by Ida program provides professional development in the core principles of PCC
SPEAKER BIO: Ena Nielsen, Associate Director & Helle Gjønnes Møller, Communications Specialist and Project Manager at the Ida Institute
 Ena Nielsen is Associate Director at the Ida Institute, a non-profit organization based in Denmark with the mission to build a community that embraces person-centered care and empowers people to get the hearing care they need. Before joining the Ida Institute, Ena worked in corporate social responsibility and strategic professional development at Deloitte for 11 years and prior to that in educational publishing. Ena holds an M.A. in German and English language and literature from the University of Copenhagen and a Ph.D. in German literature from the University of Oxford. Ena can be contacted at enni@idainstitute.dk
Ena Nielsen is Associate Director at the Ida Institute, a non-profit organization based in Denmark with the mission to build a community that embraces person-centered care and empowers people to get the hearing care they need. Before joining the Ida Institute, Ena worked in corporate social responsibility and strategic professional development at Deloitte for 11 years and prior to that in educational publishing. Ena holds an M.A. in German and English language and literature from the University of Copenhagen and a Ph.D. in German literature from the University of Oxford. Ena can be contacted at enni@idainstitute.dk
 Helle Gjønnes Møller is Communications Specialist and Project Manager at the Ida Institute. One of Helle’s key focus areas is driving the Inspired by Ida program, helping to ensure that person-centered care is prioritized and implemented in clinician practice. Helle can be contacted at hegj@idainstitute.dk
Helle Gjønnes Møller is Communications Specialist and Project Manager at the Ida Institute. One of Helle’s key focus areas is driving the Inspired by Ida program, helping to ensure that person-centered care is prioritized and implemented in clinician practice. Helle can be contacted at hegj@idainstitute.dk
FREE for all – Click to Watch Now
- Archived Webinar: Neural Correlates of Listening Effort with Andrew Dimitrijevic – Aired April 29, 2022
Aired: Friday, April 29th – 1 PM ET
SPEAKER: Andrew Dimitrijevic, PhD, Research Director of the Cochlear Implant Program at Sunnybrook Health Sciences Centre. Associate Professor University of Toronto, Dept. Otolaryngology and Physiology.
, CAA Members View the Recording - log in to view
Abstract:
Understanding the neural mechanisms of listening effort has become a “hot topic” in recent years at both clinical and basic science research levels. Clinicians have a vested interest in understanding listening effort since most of their clients seek help to resolve effortful listening to speech in real-world environments. From a basic science perspective, understanding how the brain encodes, decodes sounds and generates a subjective percept is of profound interest with applications well beyond audiology.
In this webinar we will summarize how we characterize listening effort and some physiological measures including reaction times, pupillometry, functional magnetic resonance imaging (fMRI) and electroencephalography (EEG). Special emphasis will be placed on EEG since, in my opinion, this is the most direct brain measure of listening effort. The webinar will draw upon reports of typical hearing and hearing-impaired populations including those with hearing aids and cochlear implants. Although there is still much work to be done in this relatively young field, the attendees will appreciate that listening effort is a phenomenon that can be quantified with neural metrics. Listening effort is part of many different scales/subscales of Quality of Life. Attendees will also learn that there are emerging methods to quantify Quality of Life and how we need to move beyond the audiogram to get a more complete picture of hearing.
Learning Points:
1. How can we quantify listening effort using objective measures?
2. What types of EEG signals should we look for, how do we extract these measures?
3. Can we quantify Quality of Life using neural measures?
SPEAKER BIO: Andrew Dimitrijevic, PhD, Research Director of the Cochlear Implant Program at Sunnybrook Health Sciences Centre. Associate Professor University of Toronto, Dept. Otolaryngology and Physiology.
Dr. Dimitrijevic’s work focuses on using EEG measures to understand the neural mechanisms of hearing and how hearing loss affects sensory and cognitive processing. Current themes of research include listening effort, neural metrics of quality of life, cognitive systems in audition, and neural-based rehabilitation in people with cochlear implants. Dr. Dimitrijevic completed his PhD at the University of Toronto under the supervision of Dr. Terrence Picton. His PhD examined how ASSRs (auditory steady-state responses) can be used in to objectively quantify degree of hearing loss. After his PhD, Dr. Dimitrijevic worked with Dr. David Stapells at UBC as a postdoc studying neural metrics of spatial hearing. Soon after, Dr. Dimitrijevic travelled to University of California, Irvine to work with Dr. Arnold Starr to develop objective measures in people with Auditory Neuropathy. In 2012 Dr. Dimitrijevic started a scientist position at Cincinnati Children’s Hospital Medical Centre and since 2016, Dr. Dimitrijevic has been at Sunnybrook as Research Director of the Cochlear Implant Program. www.cibrainlab.com
, CAA Members View the Recording - log in to view
- Archived Webinar: Unilateral Hearing Loss in Children: Progress and Opportunities with Anne Marie Tharpe – Aired November 2, 2022 at 1pm ET
 DATE: Wednesday, November 2, 2022 – 1 pm EST
DATE: Wednesday, November 2, 2022 – 1 pm EST
SPEAKER: Anne Marie Tharpe, Ph.D. Professor and Chair, Vickie and Thomas Flood Endowed Chair in Hearing & Speech Sciences, Department of Hearing & Speech Sciences Vanderbilt University Medical Center and School of Medicine
Abstract:
For decades, audiologists, speech-language pathologists, teachers, early interventionists, and parents have puzzled over the impact of unilateral hearing loss on children. After all, it is reasonable to assume that one normal hearing ear ought to be sufficient for hearing speech and developing language. Nonetheless, a growing body of evidence suggests that, on average, children with unilateral hearing loss have more academic, speech and language, and social-behavioral difficulties than their normal hearing peers.
This presentation will review what we know and what we do not yet know about children with unilateral hearing loss. Specifically, several theories for why these children experience difficulties will be explored and current best practices for management will be addressed. Tools intended to enhance our care of these children will be described, including those designed to address listening effort and fatigue. Research designed to inform our future management directions with these children will be discussed.
Learning Points:
Following this presentation, participants will be able to:
- List 2 challenges experienced by children with unilateral hearing loss
- List 3 hearing technologies designed to assist the listening of children with unilateral hearing loss01
- Define listening-related effort and fatigue.
SPEAKER BIO: Anne Marie Tharpe, Ph.D. Professor and Chair, Vickie and Thomas Flood Endowed Chair in Hearing & Speech Sciences, Department of Hearing & Speech Sciences Vanderbilt University Medical Center and School of Medicine
Dr. Anne Marie Tharpe is Professor and Chair, Department of Hearing and Speech Sciences, Vanderbilt University Medical Center and School of Medicine. She served as a clinical audiologist working with children with hearing loss and their families for 14 years before turning to a research career. Specifically, she has explored behavioral auditory assessment approaches, developmental impacts of minimal and mild hearing loss on children, interventions for children with hearing loss and additional disabilities and, more recently, the use of hearing technologies in the homes of children with hearing loss and children with autism spectrum disorder. Although her current administrative role consumes much of her time, she continues running a research laboratory and teaching graduate students at Vanderbilt about issues related to childhood hearing loss. Her current research is funded by the National Institutes of Health and the hearing technology industry. She also has several training grants from the U.S. Department of Education, is faculty for Vanderbilt’s Leadership Education in Neurodevelopmental Disabilities (Maternal Child Health Bureau), and has contracts with the Tennessee Department of Health, Early Intervention Services. Dr. Tharpe has over 100 publications and has spoken with more than 300 audiences around the world on various aspects of childhood hearing loss.
- Archived Webinar: CAA Clinical Placement Webinar – Aired April 19th, 2022
4CAA has assembled a talented panel of Audiologists from diverse practice areas to discuss their experiences working with students and answer all of your questions on obtaining the ideal clinical placement for your interests.
Aired: Tuesday, April 19that 8pm (EST)
FREE to students – Watch the Recording Now
Clinical Placement Webinar – CAA final 2022
Hosts: Dr. Justyn Pisa, Health Sciences Centre, Winnipeg, MB and Dr. Chris Allan, Western University, London, ON
Panelists:
- Jillian Price, M.Sc, Aud (C), HearingLife Canada & CAA Board Member
- Bonnie Cooke, MClSc, Hotel Dieu Hospital in Kingston, ON
- Salima Jiwani, Ph.D., M.Sc., AudioSense, Toronto, ON
- Daniela Stangherlin, Au.D., Central Speech and Hearing Clinic, Winnipeg, MB




- Archived Webinar: New electrophysiological methods to assess hearing function in young children using engaging stories with Melissa Polonenko – Aired March 23, 2023 at 12pm ET
3DATE: Thursday, March 23, 2023 – 12 PM ET
SPEAKER: Melissa Polonenko, Assistant Professor, Department of Speech-Language-Hearing Sciences, University of Minnesota
Abstract:
Speech is a dynamically complex sound that is essential for infants and young children to hear during their early years to support spoken language acquisition. Therefore, it is important that we identify hearing loss and other hearing challenges as soon as possible so that we can promptly provide intervention to ensure children receive an adequate representation of the speech that they need to hear. Yet current hearing tests for young children do not use continuous speech and almost a year passes before a child begins to talk or can reliably participate in speech testing. And even then, testing awake children older than 6 months can be challenging and often yields incomplete assessments. This presentation will discuss the new auditory brainstem response (ABR) test that uses narrated stories and explore the new applications for evaluating hearing function, screening for hearing loss and validating hearing aids, and evaluating speech in noise.
Learning Points:
- Many hearing skills develop in early childhood but we usually have to wait until children are able to talk and perform longer behavioral testing before we can assess these skills.
- Electrophysiological measures that use continuous speech can be measured and may provide insights into hearing function during development and in more complex environments than our traditional objective measures.
- Having audiobook-based ABR tests may provide useful information for screening hearing loss and validating hearing aids in young children in the future.
SPEAKER BIO: Melissa Polonenko, Assistant Professor, Department of Speech-Language-Hearing Sciences, University of Minnesota
Dr. Melissa Polonenko is an Assistant Professor in the Department of Speech-Language-Hearing Sciences at the University of Minnesota. She worked as an Audiologist in Edmonton Alberta before pursuing her PhD from the University of Toronto at SickKids Hospital, where she investigated outcomes in children with asymmetric hearing loss and single-sided deafness who received a cochlear implant. She developed new objective methods to assess hearing during her postdoctoral training at the University of Rochester. Her current research focuses on auditory development in children with hearing loss who use hearing aids and cochlear implants, auditory-visual integration following hearing or vision loss, and new electrophysiological paradigms to assess hearing function.
- Archived Webinar: Auditory scene analysis: understanding the fundamental mechanisms of auditory perception and perspective for audiological rehabilitation – Aired June 9, 2022 at 2pm ET
 Date: Thursday, June 9th – 2pm EST
Date: Thursday, June 9th – 2pm EST
SPEAKER: Andréanne Sharp, M.P.A., Ph.D.Professeure adjointe et Chercheure CERVO, Programme d’Audiologie, Département de réadaptation, Faculté de Médecine Université Laval
, CAA Members View the Recording - log in to view
Abstract:
In everyday life, it is rare to find an environment where there is only one sound at a time. The daily auditory scene of human is made of a wide variety of sounds with various spectral and temporal components. The ability to integrate auditory inputs that belong together and segregate those that come from different sound sources to allow a mental representation is called auditory scene analysis (Bregman, 1994).
In this webinar, you will learn what types of behavioral tasks can be used to investigate the auditory scene analysis. Auditory illusions are precious tools to better understand perception as they allow us to investigate the limits of auditory perception. In the first part of the presentation, I will discuss how auditory illusions can provide a better understanding of auditory scene analysis in difficult contexts and how these illusions can be used for research and clinical purposes.
In the second part of this webinar, a new therapeutical perspective to try to improve auditory scene analysis will be presented. A population particularly bothered by auditory scene analysis difficulties are the elderly. Age-related hearing loss is a significant problem that leads to difficulty understanding speech in noise and impaired perception of music. In a recent literature review from our laboratory, we assessed if musical therapy could be a useful tool for audiological rehabilitation in the elderly. We will discuss the reviewed evidence and perspectives for research and clinical practice in audiology.
Learning Points:
- To understand better what is auditory scene analysis and why is it so important in everyday life.
- How auditory illusions can help us to investigate auditory scene analysis?
- How can we help our patient to improve auditory scene analysis by widening horizons to to new forms of audiological therapy.
SPEAKER BIO: Andréanne Sharp, M.P.A., Ph.D.Professeure adjointe et Chercheure CERVO, Programme d’Audiologie, Département de réadaptation, Faculté de Médecine Université Laval
Andréanne Sharp is an assistant professor at Laval University in the rehabilitation department of the faculty of medicine and also, a certified clinical audiologist. Passionate about research and filled with a deep desire to improve quality of life of people with hearing loss, she obtained her Ph.D. in the Auditory Neuroscience Research Laboratory of Professor François Champoux at the University of Montreal. She then pursued postdoctoral studies in the laboratory of Dr. Robert Zatorre at McGill University. It is her musical background that gave her the innovative idea of developing research projects linking audiology and music. In her clinical practice in audiology throughout Quebec, she has met many patients complaining of difficulty perceiving music with their hearing aids. She therefore saw the need to develop new rehabilitation tools for this population. According to her, the solution to this problem began with exploration of other senses. This is why she started to develop vibrotactile technological tools allowing her to study musical perception in individuals with profound deafness.
Within her laboratory, Andréanne Sharp hopes to continue the development of knowledge in the field of adult rehabilitation by studying the limitations caused by deafness in terms of communication and recreation. To do this, the first part of his research program consists in studying the fundamental mechanisms of auditory scene analysis and music perception in normal individuals as well as those who have followed musical training. This new fundamental knowledge is necessary to develop new rehabilitation tools that can be used by clinicians. The second part of her research program aims to study the impact of deafness on auditory skills related to music perception in order to propose rehabilitation tools. She would like to investigate how to more adequately adjust existing compensatory tools for individuals with deafness (hearing aid or cochlear implant) and work on the development of new technological rehabilitation tools (for example, vibrotactile aids) in order to allow people with hearing loss to make a better analysis of the auditory scene. The professor also wishes to measure the effect of auditory training (for example, musical training) on central auditory skills in order to develop tools that can be used in rehabilitation.
, CAA Members View the Recording - log in to view
- Archived Webinar: Cognitive neuroscience of tinnitus with Fatima Husain – Aired April 26, 2023 at 1pm ET
 DATE: Wednesday, April 26, 2023 – 1 PM ET
DATE: Wednesday, April 26, 2023 – 1 PM ET
SPEAKER: Fatima Husain, Professor & Director of Undergraduate Studies, Department of Speech and Hearing Science, University of Illinois
Abstract:
Despite being fairly prevalent, tinnitus remains a mystery. In my lab and other centers around the world, brain imaging in humans is unpacking some of that mystery. In particular, it has revealed that large-scale networks, not just the auditory pathways or the primary auditory cortex, mediate the condition of tinnitus. This is not surprising given that tinnitus is both the perception of the sound and the psychological reaction to it. Brain imaging studies have also revealed how these networks change due to an intervention, such as the use of amplification or mindfulness-based training. In this lecture, I will review what we know of the extra-auditory networks implicated in tinnitus, including those known for attention and emotion processing.
Learning Points:
- The attendee will learn about both perception and psychological reaction of tinnitus sounds and how they exist on a continuum.
- The attendee will learn about how brain imaging, specifically functional magnetic resonance imaging or fMRI, is helpful in understanding the neural networks of tinnitus.
- The attendee will learn about the changes in brain networks due to an intervention such as amplification or mindfulness-based training.
SPEAKER BIO: Fatima Husain, Professor & Director of Undergraduate Studies, Department of Speech and Hearing Science, University of Illinois
Dr. Fatima T. Husain is a Professor in the Department of Speech and Hearing Science, University of Illinois Urbana-Champaign. She is also affiliated with the Neuroscience Program and the Beckman Institute for Advance Science and Technology. Dr. Husain’s research program is centered around three major themes: (1) normal audition and speech perception, (2) disorders of the auditory system, particularly hearing loss and tinnitus, and (3) effects of aging on audition and cognition. She uses a multidisciplinary approach combining behavioral, brain imaging, and computational neuro-modeling tools. She has published over 38 peer-reviewed journal articles on tinnitus and neural bases of tinnitus.
- Archived Webinar: Communication strategies to support client behaviour change with Jennifer Irwin – Aired June 3, 2021
DATE: Thursday, June 3rd – 2 PM ET
SPEAKER: Dr. Jennifer Irwin, Health Behaviourist, The Monarch System, Inc.
Abstract:
Do you ever feel like you are more invested in your clients’ health-related behaviours than they are? Or, that you spend a fair amount of energy trying to convince clients to do what’s in their best interest? Do you wish there were some fairly simple tools to help facilitate your clients feeling and being more invested in their own changes? There are! This brief introductory webinar brings aspects of motivational interviewing, coaching, and health behaviour theory together to focus on some practical, evidence-based communication strategies to help build motivation and transition that enhanced motivation into a strengthened and real commitment to behaviour change.
Learning Points:
By the end of this talk, participants should have a basic understanding/review of:
- some evidence-based, effective ways to communicate with clients to foster behaviour change;
- how “not to” communicate with clients, if the goal is behaviour change; and
- how effective communication with clients benefits both clients and providers.
Speaker: Dr. Jennifer Irwin, Health Behaviourist, The Monarch System, Inc.
Dr. Jennifer Irwin is a health behaviourist, motivational interviewing and coaching trainer, multi-award-winning teacher, and widely published researcher. With 100+ peer-reviewed journal articles, 5 books, and 130 invited talks, Dr. Irwin is most proud of her collaborative work with those who are working to make our world a healthier and better place. She is passionate about kindness, collaboration, and each of us doing our part to support one another. Her research focusses primarily on the application of motivational interviewing and coaching on health-related behaviours.
 DATE: Wednesday, September 28, 2022 – 12pm EST
DATE: Wednesday, September 28, 2022 – 12pm EST
SPEAKER: Marlene Bagatto, Au.D., Ph.D., Assistant Professor, School of Communication Sciences and Disorders and the National Centre for Audiology, at Western University.
CAA Members view the recording (must login first)
Non Member fee – $50.00
Abstract:
Audiologists who support children who have hearing loss regularly encounter challenging cases. For these unique scenarios, the various assessment and management protocols that are available may not provide the guidance we need. This is because the main goal of clinical protocols is to provide the necessary details to operationalize the evidence-based guidance on best practice for the target population. Protocols do not and cannot address the unique characteristics of the child, family, and clinical and environmental contexts. Further, research questions remain unanswered for many of the situations we face as pediatric audiologists. Regardless, we are motivated to apply the protocol and our best clinical judgement to make recommendations for the child and family. When clinical uncertainty arises due to the state of knowledge about the scenario, this is known as “clinical equipoise”. This concept is helpful as we navigate these challenging scenarios.
In this presentation, pediatric case examples will be shared for discussion. Each case will have its own challenging characteristics that are not addressed by current research or protocols. Attendees will learn about the clinical recommendations and resulting outcomes for each case. It is anticipated that more questions than answers will surface as a result of this presentation.
Learning Objectives:
- Describe the challenges associated with managing unilateral hearing loss in infants.
- Explain some factors when considering technology recommendations for infants and young children who have auditory neuropathy spectrum disorder (ANSD).
- Define how to proceed with a hearing aid fitting to an infant who has no responses to the auditory brainstem response (ABR) assessment.
SPEAKER BIO: Marlene Bagatto, Au.D., Ph.D., Assistant Professor, School of Communication Sciences and Disorders and the National Centre for Audiology, at Western University.
Marlene Bagatto is an Assistant Professor in the School of Communication Sciences and Disorders and the National Centre for Audiology at Western University. The research in her Pediatric Audiology Strategies and Systems Laboratory focusses on policy and practice integration for infant and child hearing. Dr. Bagatto is Chair of the Canadian Infant Hearing Task Force which advocates for equitable infant hearing health care across Canada. Marlene is a Past President of CAA, and a CAA Board Member.
CAA Members view the recording (must login first)
Non Member fee – $50.00
- Archived Webinar: Communication Access for Children Via Personal Remote Microphone Systems: What Does Research Tell Us? With Dawna Lewis – Aired June 29, 2021

SPEAKER: Dawna E. Lewis, PhD, Senior Research Associate, Boys Town National Research Hospital, Omaha, Nebraska
Abstract:
The negative effects of noise, distance, and reverberation on children with hearing loss have been well-documented. In many situations, hearing instruments alone are not sufficient to allow communication access for these children across a range of environments. Research also has shown that children with normal hearing and special listening needs can be negatively impacted by poor acoustics. Remote microphone systems are designed to overcome the deleterious effects of noise, distance, and reverberation. In the 1960s, self-contained remote microphone systems using frequency modulation (FM) technology and body-worn receivers were first introduced. Advances in remote microphone technology have continued to improve their flexibility, adaptability, and convenience. Although ongoing advances in hearing-instrument technology also have resulted in improved speech understanding for listeners with hearing loss, use of remote microphone systems remains an important option for speech understanding in complex acoustic environments. This seminar will provide attendees with a discussion of research on personal remote microphone technology for children as it relates to their communication access. Future research needs to continue to advance our evidence base also will be addressed.
Learning Points:
- Have knowledge of advances in personal remote microphone technology since its introduction in the 1960s.
- Have knowledge of the impact of remote microphone technology on speech understanding in children with hearing loss and in children with normal hearing who have special listening needs.
- Have knowledge of research findings regarding remote microphone technology.
Speaker: Dawna E. Lewis, PhD, Senior Research Associate, Boys Town National Research Hospital
Dawna Lewis, PhD, is a Sr. Research Associate at Boys Town National Research Hospital in Omaha, Nebraska. She has presented and published on topics involving pediatric audiology/amplification and hearing assistance technologies, including remote microphone systems. Dr. Lewis served on the AAA Task Force on Guidelines for Remote Microphone Hearing Assistance Technology. She is involved in research addressing issues related to amplification and speech perception in children. Recent work has examined the impact of mild bilateral and unilateral hearing loss on children’s speech understanding in complex environments by manipulating acoustic and visual characteristics of the environments and tasks.
- Archived Webinar: Addressing the elephant in the room: sales in a clinical profession with Andreas Seelisch – Aired April 22, 2021
DATE: Thursday, April 22nd– 1 PM ET
SPEAKER: Speaker: Andreas Seelisch, M.Sc., B.H.Sc. (Hons), Reg. CASLPO , Director of Audiology, Hearing Solutions
Abstract:
Many clinicians enter audiology unaware that sales acumen was something they might need. Whether it’s not an interest, does not come naturally or was wasn’t a part of their formal education, it does remain a very real part of private practice. This evidence based talk addresses some of the aspects of our profession that make many of us uncomfortable such as talking about money, hearing aids being expensive and other common objections we face when counselling with our patients.
This talk will address reconciling what it means to be both a medical professional as well as a salesperson and how that doesn’t need to be a conflict. We will identify a variety of practical tools and strategies for clinicians to choose from that can organically compliment their individual style and ultimately help achieve success in reaching more patients while feeling good about it! Finally it covers what the literature tells us about some of the most common objections and how we can use that understanding to help manage those objections better.
- Help reconcile what it means to be an audiologist as well as a sales professional
- Discuss common objections, what they mean and how to manage them
- Provide tools and strategies that help us better understand and connect to our patients
Speaker: Andreas Seelisch, M.Sc., B.H.Sc. (Hons), Reg. CASLPO , Director of Audiology, Hearing Solutions
Andreas Seelisch is the Director of Audiology at Hearing Solutions, the largest independently owned and operated hearing aid retailer in Ontario. He graduated from Western University with a Masters in Communication Sciences and Disorders in 2008 and completed his thesis work at the National Centre for Audiology on the sound quality impact of frequency compression technology. His current research focus is on clinically applicable topics such as clinical practice guidelines and exploring barriers to hearing aid uptake.
- Archived Webinar: Audibility-based hearing-aid candidacy for children with Ryan McCreery – Aired December 1, 2020
DATE: Tuesday, December 1st -1 PM ET 
SPEAKER: Ryan McCreery, Ph.D. Director of Research, Director of the Audibility, Perception, and Cognition Laboratory, Boys Town National Research Hospital
Abstract:
Audiologists often rely on the dB HL audiogram to make decisions about hearing-aid candidacy for children. However, this approach leads to inconsistencies in when hearing aids are recommended, particularly for children with mild or minimal hearing losses. The goal of this presentation is to discuss the rationale and supporting data for a hearing-aid candidacy based on the child’s unaided speech audibility. The presentation will include a review of the variability in outcomes for children with mild bilateral hearing loss in previous research and a clinical protocol for supporting hearing-aid candidacy decisions for children with estimates of unaided audibility.
Learning Points:
1. Discuss the limitations of the dB HL audiogram as it relates to estimating speech audibility for children.
2. Implement an audibility-based approach to hearing-aid candidacy for children.
3. Describe the caveats to using an audibility-based hearing-aid candidacy criterion
SPEAKER BIO: Ryan McCreery, Ph.D. Director of Research, Director of the Audibility, Perception, and Cognition Laboratory,
Boys Town National Research Hospital
Ryan McCreery is the Director of Research and Director of the Audibility, Perception, and Cognition Laboratory at Boys Town National Research Hospital in Omaha, NE. Ryan provides strategic leadership to the 6 centers and 26 laboratories that comprise the BTNRH research program. His NIH-funded research examines the effects of hearing loss and cognitive development on speech perception in children with typical hearing and children with hearing loss.
- Archived Webinar: Psychological Factors Associated with Hearing Aid Adoption With Gurjit Singh – Aired November 24, 2020
 DATE: Tuesday, November 24th – 1 PM ET
DATE: Tuesday, November 24th – 1 PM ET
SPEAKER: Gurjit Singh, PhD, reg. CASLPO Senior Research Audiologist, Phonak Canada, Adjunct Professor, University of Toronto; Ryerson University
Abstract:
Hearing loss is a highly prevalent and significantly disabling health condition, and the most common treatment is the provision of hearing instruments. Despite the availability of evidence supporting positive health outcomes associated with hearing instrument use, hearing aid adoption rates remain low. Why is this the case? Research investigating factors that contribute to hearing aid adoption focuses mostly on the role of personal factors (i.e., degree of audiometric hearing loss, personality, attitude, etc.) and demographic factors (i.e., age, gender, etc.), and only focuses somewhat on the role of external factors (i.e., cost, counselling, etc.). Critically, there has been an under-emphasis on understanding how interpersonal and contextual factors contribute to hearing aid adoption. This is somewhat surprising given decades of research on decision-making processes from other fields such as social and cognitive psychology. This presentation will consist of a brief theoretical review of frameworks relevant to better understand decision-making processes, a review of how modern data acquisition techniques can inform hearing rehabilitation research, a review of several large-scale studies investigating hearing aid adoption and associated hearing rehabilitation outcomes, and several concrete ‘takeaways’ designed to inform clinical practice.
Learning Points:
- Attendees will be exposed to information about models of behaviour change.
- Attendees will be exposed to examples of family-centred care practices.
- Attendees will be exposed to research on the role of emotion in hearing rehabilitation
SPEAKER BIO: Gurjit Singh, PhD, reg. CASLPO Senior Research Audiologist, Phonak Canada, Adjunct Professor, University of Toronto; Ryerson University
Dr. Gurjit Singh works as a researcher in the long-term research division of Sonova AG. In addition to being a clinical audiologist, he completed degrees in social psychology focused on decision-making and a PhD in cognitive psychology. His research interests focus on factors that lead to success with hearing rehabilitation.
- Archived Webinar: Measuring and Understanding Tinnitus – including patients views on the ‘Meaning of Life’ With Richard S. Tyler – Aired November 19, 2020
DATE: Thursday, November 19 -7 PM ET 
SPEAKER: Richard S. Tyler, Professor, Tinnitus Clinic Director, Department of Otolaryngology, The University of Iowa
Abstract:
It is important to distinguish the tinnitus from the reactions to the tinnitus. We have referred to this as our “Psychological Model”. The reactions are also influenced by our individual live experiences and our psychological make-up. The tinnitus can be measured with loudness ratings and the minimum masking level. The reactions can be measured with the Tinnitus Primary Functions Questionnaire. Everyone is different, but the common reactions are 1) thoughts and emotions, 2) hearing, 3) sleep and 4) concentration. Tinnitus Activities Treatment addresses these individual differences. We have compared the Meaning of Life in tinnitus and cochlear implant patients.
Learning Points:
1. Understand the challenges faced by tinnitus patients
2. Learn strategies to show them you care and want to be helpful
3. Appreciate the significance of hearing difficulties and hearing a sound you have no control over
SPEAKER BIO: Richard S. Tyler, Professor, Tinnitus Clinic Director, Department of Otolaryngology, The University of Iowa
Richard received a B.Sc. (Communication Disorders) and a M.Sc. (Audiology), at the University of Western Ontario. He then received a Ph.D. in Psychoacoustics from the University of Iowa. He is currently a Professor in Otolaryngology and in Communication Sciences and Disorders at the University of Iowa. Richard has been a visiting scholar in China, South Africa, Australia, Sweden, Poland, Germany and France. He was made an Honorary Professor in The Society of Medicine and Natural Science, at the University of Parma, Italy, (2016) for my contributions to the Cochlear Implant field. His main areas of interest include tinnitus, hyperacusis and cochlear implants. He edited, Cochlear Implants: Audiological Foundations, the Tinnitus Handbook, Tinnitus Treatments, and A Consumer Handbook of Tinnitus. Richard has served on several grant review committees for NIH, VA, DOD and others. He has served on committees for the National Science Foundation, the World Health Organization, the Department of Defence, the American Academy of Otolaryngology, and the Veterans Administration. He sees tinnitus patients weekly, and hosts an annual Tinnitus and Hyperacusis Treatment Workshop every June.
- Archived Webinar: Therapeutic Techniques for Counseling Complex Patients with Hearing Challenges and Their Families With Michael Hoffman – Aired November 12, 2020
DATE: Thursday, November 12th – 7 PM ET
SPEAKER: Michael Hoffman, PhD, Pediatric Psychologist, Nemours/AI duPont Hospital for Children
Abstract:
This presentation will review counselling techniques that can be used during interactions with complex patients and their families. This includes specific techniques taught to psychologists that can increase patients/family engagement, elicit additional information, and facilitate problem-solving for common difficulties, including limited hearing aid usage, adjustment to a new diagnosis of hearing loss, and family disagreement with medical recommendations. Time will also be spent reviewing the role of diversity, multicultural identity, and cultural humility during patient interactions. Finally, strategies such as motivational interviewing will be modeled during case examples to highlight the counselling techniques. Overall, this seminar will provide attendees with clear, specific ways to navigate complex patient interactions and potentially facilitate better outcomes.
Learning Points:
1. Review specific techniques that can be used to increase patient satisfaction and engagement during appointments
2. Present a model for considering the role of multicultural identity and its impact on patient interactions
3. Highlight therapeutic techniques using case examples
SPEAKER BIO: Michael Hoffman, PhD, Pediatric Psychologist, Nemours/AI duPont Hospital for Children
Dr. Michael Hoffman is a Pediatric Psychologist at Nemours/AI duPont Hospital for Children who specializes in working with children with chronic medical conditions. Dr. Hoffman’s clinical work centers on children with hearing differences, related hearing disorders, and cleft palate/craniofacial differences. This includes meeting with families who receive a new diagnosis of hearing loss, those going through the cochlear implant evaluation process, managing challenges related to anxiety, depression, and deaf identity, and reducing barriers to limited device usage. Dr. Hoffman’s research focuses on integrating psychological services into Audiology/ENT clinics and improving quality of life in children and adolescents with hearing differences. Dr. Hoffman is also a deaf individual, utilizing one cochlear implant and one hearing aid.
- Archived Webinar: Hearing and Balance: Impact and Outcomes of Dual Sensory Impairments in the Pediatric Population With Sharon Cushing – Aired October 20, 2020
DATE: Tuesday October 20 -7 PM ET
SPEAKER: Sharon L. Cushing MD MSc, FRCSC, Otolaryngologist, Hospital for Sick Children
Abstract:
Sensorineural hearing loss (SNHL) in children occurs in 1-3% of live births and acquired hearing loss can additionally occur. This sensory deficit has far-reaching consequences that have been shown to extend beyond speech and language development. Thankfully there are many therapeutic options that exist for these children with the aim of decreasing the morbidity of their hearing impairment. Of late, focus has shifted beyond speech and language outcomes to the overall performance of children with SNHL in real world environments. To account for their residual deficits in such environments, clinicians must understand the extent of their sensory impairments.
Increasingly, SNHL is considered to commonly co-exist with other sensory deficits such as vestibular loss. It is known that vestibular impairment is exceedingly common in children with SNHL with nearly half of children exhibiting vestibular end-organ dysfunction. These deficits naturally lead to impairments in balance and delay in motor milestones. However, this additional sensory deficit likely leads to further impairment in the performance of these children. Attendees of this webinar will come away with a better understanding of the sensory contributions that impact outcomes in the children we care for with hearing loss.
Learning Points:
- Defining the co-existence of vestibular impairment in children with SNHL and cochlear implants (CI)
- Describing screening methods aimed at identifying vestibular dysfunction in children with SNHL
- Understanding the functional implications of this dual sensory impairment
- Exploring possible rehabilitative strategies to minimize the impact of vestibular impairment in children with SNHL
SPEAKER BIO: Sharon L. Cushing MD MSc, FRCSC, Otolaryngologist, Hospital for Sick Children
Dr. Sharon Cushing is a full time paediatric otolaryngologist at The Hospital for Sick Children in Toronto, Canada, and an Associate Professor and Clinician Investigator in the Department of Otolaryngology Head and Neck Surgery at the University of Toronto. She is the Director of the Cochlear Implant Program at the Hospital for Sick Children. Dr. Cushing has a clinical and surgical interest in disorders of the external, middle and inner ear, including hearing loss and vestibular dysfunction. Her research interest include vestibular and balance function and dysfunction in children, and its association with hearing loss and cochlear implantation.
Dr. Cushing completed her undergraduate degree at Queen’s University in Kingston, followed by Medical School and Residency training in Otolaryngology Head and Neck Surgery at the University of Toronto. In addition, Dr. Cushing completed a Master’s in Science degree examining vestibular function and balance in children with hearing loss through the Surgeon Scientist Program at the University of Toronto. She completed her fellowship training in Paediatric Otolaryngology at Seattle Children’s Hospital prior to returning to Sick Kids in Toronto.
- Archived Webinar: Personal Protection Equipment and Individuals with Hearing Loss: The Impact on Communication – Aired June 23, 2020
 Aired: Tuesday, June 23
Aired: Tuesday, June 23
Speaker: Dr. Dave Gordey, Past President of CAA, Oticon
Abstract: COVID-19 has prompted the use of face masks and shields in community spaces. For individuals with hearing loss, the impact of face masks on communication can be very challenging. When combined with imperfect listening environments, the use of face masks and shields may further degrade the speech signal and restrict access to visual cues. Research has shown face masks/shields can impact audibility for those who wear hearing technology, behaving like a filter for high frequencies (Goldman, Weinstein & Shiman, 2020). For children with hearing loss returning to school, it is likely they may encounter teachers and other school-based professionals who will be using personal protective equipment (PPE). The aim of this project was to evaluate the effect of different PPE on audibility for students with hearing loss.
Speaker Bio: Dave Gordey, Ph.D., Past President of CAA, Director, Oticon A/S
Dave Gordey has been a pediatric audiologist for twenty-seven years. Dave previously worked in a pediatric clinic and hospital in Victoria and North Vancouver. Dave is the director of pediatric audiology and research for Oticon A/S in Copenhagen, Denmark, and is the past president of the Canadian Academy of Audiology. Dave has taught at York University and at the University of British Columbia. Dave’s current research projects include pediatric hearing aids, bone conduction devices and children, unilateral hearing loss, the social and emotional development of children with hearing loss, and knowledge translation and implementation science in pediatric audiology.
- Archived Webinar: Employment Law Considerations for Employers Re-opening their Audiology Business Post COVID-19 with Anthony Panacci – Aired June 4, 2020
CAA Members watch the recording now
CAA Members Read the Article – Employment Law Considerations for Employers Re-opening Your Audiology or Hearing Health Business
Aired: Thursday June 4th at 12 pm ET
Speaker: Anthony Panacci, Lawyer, Filion Wakely Thorup Angeletti LLP, presents Employment Law Considerations for Employers Re-opening their Audiology Business Post COVID-19 Webinar.
ABSTRACT: While provinces continue to operate under a state of emergency, audiology businesses are proactively planning for the resumption of business operations and the return of workers to the physical workplace. Businesses need to plan for the “new normal” in a post-pandemic era. We invite you to join us for a webinar that will help employers identify, and effectively manage, issues related to the reopening of the economy amidst the ongoing threat of COVID-19.
The webinar will address:
- Ongoing health and safety obligations related to COVID-19
- Recalling employees to work, in both unionized and non-unionized workplaces
- Managing employees who will not or cannot return to work when scheduled
Speaker: Anthony Panacci, Lawyer
Anthony Panacci is a lawyer with Filion Wakely Thorup Angeletti LLP, is one of Canada’s leading management-side labour and employment law firms. Anthony provides advice to both unionized and non-unionized organizations on all aspects of the employment relationship. This includes helping employers with the hiring process, terminations, health and safety matters, and employment policies. He regularly advises employers and defends employers in legal proceedings.
Host: Salima Jiwani
- Archived Webinar: eAudiology Webinar – Privacy and Practicality with Bill Campbell and Erica Zaia- Aired April 30, 2020
Watch the Recording Now
eAudiology PDF
Aired: Thursday, April 30th at 1 pm ET
Speakers: Bill Campbell, Audiologist and Erica Zaia, Audiologist
eAudiology as a tool to reach patients who may find it challenging to access an audiology clinic in person has gained notoriety recently, due in part to the coronavirus crisis. Clinicians who wish to implement eAudiology components in their practice are challenged by the confusing tangle of layered privacy legislation. Gaining a complete understanding of relevant privacy legislation and how it applies to eAudiology is a challenge even for those who have access to legal advice and other resources. The legislation as it exists today is said to be outdated, layered, and often contradictory. The degree of responsibility and liability for the clinician is dependent on outside factors.
Additionally, there are a myriad of possible solutions for eAudiology service delivery. There are videoconference and data-sharing platforms designed for eHealth, for business, and for social communication. Some are available at no cost, while some have significant fees for use. As well, some platforms are easily accessed and understood by patients, where some may be cumbersome to use. Platforms that are based in other countries may or may not be compliant with applicable Canadian privacy legislation.
This webinar is intended to assist hearing health care clinicians in navigating the privacy ‘fog’ and to make informed decisions to ensure patient confidentiality. As well, real world practical experience and solutions will be discussed. Attendees will learn:
- A completely new and different way to view your roles and responsibilities as a clinician.
- Practical suggestions for video conference and data-sharing solutions.
- Real world experience in delivering rehabilitation counseling remotely.
Speakers: William (Bill) Campbell, MCISc, eEHDI Advocate & Activist, Audiologist, a Past President of CAA and Erica Zaia, MSc, Audiologist, CAA Board Member
Host: Dr. Salima Jiwani, a Past President of CAA
All CEU webinars are valid for one CEU.
- A.T. Still University’- 20% discount
A.T. Still University’s Post-Professional Doctor of Audiology is reminding our professional organization partners that qualifying members may receive a 20% discount in tuition for non-degree seeking courses.
Upcoming courses:
Courses offered May 25, 2020-June 21, 2020:
AUDP 8410 Advanced Acoustic Immittance
AUDP 8420 Otoacoustic Emissions: Scientific Foundations and Clinical Applications
AUDP 8430 Tinnitus and Hyperacusis: Theories, Evaluation and Treatment
AUDP 8440 Occupational and Environmental Hearing Conservation
Courses offered July 13, 2020-September 13, 2020:
AUDP 7200 Pathologies of the Auditory and Vestibular System
AUDP 7300 Pharmacology & Ototoxicity
AUDP 7500 Genetics and Hearing Loss
AUDP 8200 Amplification: Assessment, Fitting, and Verification
AUDP 8210 Implantable Devices
AUDP 8220 Counseling, Aural Rehabilitation and Assistive Devices
AUDP 8600 Assessment and Management of (Central) Auditory Processing Disorders
AUDP 8700 Hearing Loss and Healthy Aging
For course descriptions, tuition, and online application, please visit our Post-Professional Doctor of Audiology Program Non-Degree Seeking website at https://www.atsu.edu/post-professional-doctor-of-audiology-non-degree#requirements
- Archived Webinar: eAudiology: For right now and for the future webinar with Bill Campbell – Aired April 2, 2020
Watch the recording now CEU credits will be issued via email in early May.
eAudiology PDF
Cyber Security Advisory – Zoom
Aired: Thursday, April 2nd, 2020 – 2 pm – 3 pm ET
Speaker: William (Bill) Campbell, MCISc, eEHDI Advocate & Activist, Audiologist, a Past President of CAA
During the COVID-19 pandemic, hearing health care clinics are either closed or providing significantly reduced services. Clinics are struggling with financial viability and will be facing appointment backlogs once normal services resume. Many audiologists are wondering if eAudiology strategies can enable them to assist patients during this difficult time. eAudiology solutions facilitate patient service with no physical contact, allowing clinicians to interact with patients to address immediate/urgent concerns, to continue patient services and to reduce future of services.
eAudiology solutions vary widely depending on clinic, patient needs and resources. Not every solution will work in a given clinic situation. It is important for audiologists to be familiar with the options available and limitations of current circumstances to choose appropriate solutions and strategies that will work for their clinic and their patients. eAudiology practices must be compliant with patient confidentiality, data security, privacy laws and infection control needs related to the pandemic.
The presentation provides a broad overview of eAudiology strategies and offers practical solutions to specific needs. Attendees will learn:
- Privacy, security, and patient confidentiality concerns and solutions.
- Three groups of eAudiology solutions and the viability of each solution in a given situation.
- Strategies for evaluating eAudiology solutions and continued use once normal clinic operations resume.
Watch the recording now
Date: Thursday, April 2nd, 2020 – 2 pm – 3 pm ET
Speaker: William (Bill) Campbell, MCISc, eEHDI Advocate & Activist, Audiologist, Past President of CAA
Bio: Voted “Most Likely to Invent Something” by his graduating audiology class at Western University in 2000, Bill Campbell has been involved in eAudiology since 2008. A regional program coordinator and audiologist for the Ontario Infant Hearing Program in Thunder Bay Ontario, Canada since 2001, Bill has worked to solve access to services barriers in remote northern Canadian communities. He has collaborated with the National Centre for Hearing Assessment and Management (NCHAM) in developing a resource guide supporting teleaudiology. Bill has also collaborated with the University of South Dakota in developing their infant teleaudiology and related training program. Although recently retired from a successful private practice in Thunder Bay, Bill continues to consult with the Ontario Infant Hearing Program on protocol development and their remote infant ABR assessment program. He is also an active member of Phonak’s “expert circle”, presently focusing on eAudiology awareness.
- Archived Webinar: Applying Person-Centered Care (PCC) in the Appointment with Cherilee Rutherford – Aired May 27, 2020
Watch the recording
PDF
This webinar will translate person-centered care from theory into practice. The Calgary-Cambridge Guides and the Four Habits provide the framework of the session. The webinar will focus on the importance of applying person-centered care throughout the appointment and the research that demonstrates the reality of what happens when it comes to “walking the talk” of PCC.
Key learning points
- Review the concept of person-centered care and define the key components of person-centered communication in hearing care and rehabilitation.
- Revisit the Calgary-Cambridge Guides and introduce The Four Habits to facilitate a person-centered interaction.
- Review key communication skills that are fundamental in any hearing care or rehabilitation scenario.
Speaker: Cherilee Rutherford, Ida Institute
Cherilee is the senior audiologist at the Ida Institute. Her professional qualifications include a Bachelors degree in Speech-Language Therapy and Audiology (University of Stellenbosch), a Masters of Health Science and a Professional Doctorate in Audiology (Nova Southeastern University (Florida) as well as Postgraduate Certificates in Teaching and Learning for Higher Education (UCL, London) and Online Facilitation (University of Cape Town). Before joining Ida, Cherilee was the course director for the MSc in Advanced Audiology programme at University College London and lectured at the University of Cape Town in amplification technology and aural rehabilitation.
The Ida Institute is a non-profit organization founded in 2007 by a grant from the William Demant Foundation.
Our mission is to build a community that embraces person-centered care and empowers people to get the hearing care they need. We work with clinicians, academics, and people with hearing loss to create resources that help people develop the knowledge, skills, and confidence to better manage hearing loss.
The Ida Institute is based in Denmark and has a community of +16,000 hearing health care professionals worldwide. Read more at idainstitute.com.
- Archived Webinar: Understanding Cases of Tinnitus with a Normal Audiogram: Is Hearing Loss Undetected with Brandon Paul – Aired June 9, 2020

Aired: Tuesday, June 9th at 12 pm ET
Speaker: Brandon Paul, PhD., Sunnybrook Health Sciences Centre
ABSTRACT: The majority of individuals with subjective chronic tinnitus exhibit shifts in the clinical audiogram that signal a degree of hearing loss. These observations support the idea that damage to structures in the ear precipitate a cascade of neuroplastic changes in the brain that give rise to the sensation of phantom sounds. However, 10–15% of individuals with tinnitus have normal hearing thresholds in both ears up to 8 kHz.
This presentation will consider potential reasons that some individuals with tinnitus have hearing thresholds within normal limits. For instance, audiometric shifts may be present but are missed by conventional testing, or damage may have occurred to sensory cells in a manner that does not affect thresholds. An emphasis will be placed on the topic of cochlear synaptopathy, a form of “hidden hearing loss” describing damage to synaptic connections between inner hair cells in the cochlea and auditory nerve fibers. The webinar concludes by describing physiological measures that may reveal synaptopathy, as well as the hurdles that remain before these tests can be used in clinical practice.
Learning points
- Standard audiometry may miss threshold shifts that are present in tinnitus sufferers, namely at frequencies above 8 kHz, or at several interoctave frequencies.
- Cochlear synaptopathy, or “hidden hearing loss,” may be present in individuals who have normal audiograms (even to 16 kHz) but chronic tinnitus.
- Detecting cochlear synaptopathy has proven difficult in humans, and thus the relationship between tinnitus and synaptopathy is unresolved.
Speaker: Brandon Paul is a Postdoctoral Fellow at Sunnybrook Research Institute and the Department of Otolaryngology within Sunnybrook Health Sciences Centre in Toronto. His research interests concern tinnitus, cochlear implant outcomes, cognitive consequences of hearing loss, and neuroimaging using electroencephalography (EEG). His research has been funded by the Natural Sciences and Engineering Council (NSERC) of Canada, and the American Tinnitus Association.
- Archived Webinar: The Importance of Vestibular Assessment in Sport-Related Concussions with Jamie M. Bogle – Aired Feb 25, 2020
Date: Tues, Feb 25, at 12 pm ET
Speaker: Jamie M. Bogle, AuD, PhD, Division Chair of Audiology, Assistant Professor of Audiology, Mayo Clinic Arizona
CAA Members Watch Now
Presentation PDF, and Return to Play Stages Handout
(remember to sign in first then select members only links)
Non CAA Members – Webinar Registration – fee $50.00
ABSTRACT: Sport-related concussion is a significant public health concern that requires a multidisciplinary team to appropriately manage. Athletes often report dizziness and imbalance following concussion. Vestibular diagnostics can provide significant information for providing appropriate management to these patients. Identifying underlying deficits related to oculomotor function, gaze stability, and balance help to appropriately refer athletes to appropriate rehabilitation services and education accommodations, but also serve as biomarkers for recovery and when it is safe for the athlete to return to play. The purpose of this presentation is to provide background on the current understanding of concussion on the peripheral and central vestibular system and to describe an abbreviated protocol useful in identification of acute injury and for monitoring recovery.
Learning Points
- To describe the importance of understanding concussion symptoms and clinical presentation
- To analyze current understanding of concussion presentation in the vestibular clinic
- To evaluate current diagnostic capabilities in evaluating concussion and concussion recovery in the vestibular clinic
Speaker: Jamie M. Bogle, AuD, PhD
Division Chair of Audiology, Assistant Professor of Audiology, Mayo Clinic Arizona
Jamie M. Bogle, AuD, PhD, is an Assistant Professor of Audiology at the Mayo Clinic College of Medicine and Science and the division chair of Audiology at Mayo Clinic Arizona. Clinically, Dr. Bogle evaluates children and adults with dizziness and imbalance due to peripheral and central conditions. She is interested in improving the diagnostic tools available for evaluating patients across the lifespan to better understand inner ear function in both typical and disordered patients. Her research interests include the integration of visual and vestibular information in individuals with neurological impairments, including concussion, and the improved understanding of the importance of vestibular gravito-inertial information into overall body function. She earned her Doctorate of Audiology (AuD) and PhD from the University of Colorado at Boulder and was awarded the James and Martha Crawford Endowed Clinical Research Fellowship in Otolaryngology at Mayo Clinic Florida. She was awarded the Outstanding Early-Career Audiologist Award in 2018 and was recently elected to the Board of Directors for the American Academy of Audiology.
CAA Members Watch Now
(remember to sign in first then select members only links)
Non CAA Members – Webinar Registration – fee $50.00
- Archived Webinar: Hearing Healthcare for Infants and Children in Canada: Status of EHDI Programs with Marlene Bagatto, Sheila Moodie – Aired April 10, 2019
Speakers: Marlene Bagatto, AuD, PhD, Aud(C) & Sheila Moodie, PhD
Presented: Wednesday, April 10th, 2019
CAA Members watch the recording now
Early hearing detection and intervention (EHDI) programs are available worldwide to proactively address hearing health in infants and children. A report card issued in 2014 from the Canadian Infant Hearing Task Force indicated that comprehensive EHDI programs were not available across Canada.
In this presentation, we will describe a status update of EHDI programs in Canada based on information gathered through a 24-item, country-wide survey. Results from this work revealed that, as a whole, Canada remains insufficient in offering comprehensive, accessible and sustainable EHDI programs. Continued action from Canada’s governments, in addition to federal policy leadership, is needed to achieve sufficient and sustainable EHDI programs.
Learning Objectives: Participants of this presentation will be able to:
- Describe the components of a comprehensive EHDI program.
- Explain the status of EHDI programs across Canada.
Level: Intermediate
This webinar is eligible for a CAA CEU. This webinar is for CAA and SAC members only.
Speakers: Marlene Bagatto, AuD, PhD, Aud(C) & Sheila Moodie, PhD
 Marlene Bagatto, AuD, PhD, Aud(C)
Marlene Bagatto, AuD, PhD, Aud(C)
Marlene Bagatto is a professor at Western University in the School of Communication Sciences and Disorders and the National Centre for Audiology. She is the chair of the Canadian Infant Hearing Task Force and was the president of the Canadian Academy of Audiology.
Sheila Moodie, PhD
Sheila Moodie is an associate professor at Western University in the School of Communication Sciences and Disorders. She is a member of the National Centre for Audiology and the Canadian Infant Hearing Task Force and is the director of the Family-Centred Early Intervention Lab at Western University.
- Archived Webinar: What the Auditory Cortex Does Before and After Hearing Loss with Stephen G. Lomber – Aired May 29, 2019
Date: Wednesday, May 29th at 1 pm ET
Speaker: Stephen G. Lomber Ph.D., Professor of Physiology and Psychology, University of Western Ontario
CAA Members Watch Now
ABSTRACT: Cortical plasticity is the neural mechanism by which the cerebrum adapts itself to its environment, while at the same time making it vulnerable to impoverished sensory or developmental experiences. Like the visual system, auditory development passes through a series of sensitive periods in which circuits and connections are established and then refined by experience. During these periods, the functional maturation of auditory processing and perception is critically dependent on adequate auditory experience. Unfortunately, in cases of sensory deprivation, such as congenital deafness, this process is arrested. Fortunately, it appears that this situation can be reversed in individuals that receive cochlear prosthetics.
Current research is expanding our understanding of cerebral processing and organization in the deaf. In the congenitally deaf, higher-order areas of “deaf” auditory cortex demonstrate significant crossmodal plasticity with neurons responding to visual and somatosensory stimuli. This crucial cerebral function results in adaptive, compensatory plasticity. Not only can the remaining inputs reorganize to substitute for those lost, but this additional circuitry also confers enhanced abilities to the remaining systems. In this presentation, we will review our present understanding of the structure and function of “deaf” auditory cortex using psychophysical, electrophysiological, and connectional anatomy approaches and consider how this knowledge informs our expectations of the capabilities of cochlear implants in the developing brain.
Learning Objectives:
- To learn how anatomical, electrophysiological, and psychophysical techniques can be used to examine the functional organization of the auditory cortex in hearing and deaf subjects.
- To learn how the absence of auditory input during brain development alters the developmental trajectory of auditory cortex and how even short periods of acoustic experience during development can have a major influence on cerebral organization.
- To appreciate how cochlear implants can re-establish an auditory cortical organization similar to that of a hearing individuals.
Speaker Bio: Stephen G. Lomber Ph.D
Stephen G. Lomber, Ph.D. is a Professor of Physiology and Psychology at the University of Western Ontario where he holds the Canada Research Chair in Brain Plasticity and Development. Steve directs the Cerebral Systems Laboratory (www.cerebralsystems.ca) and is a Principal Investigator in the National Centre for Audiology and the Brain and Mind Institute. Dr. Lomber’s lab uses an integrated approach of psychophysics, electrophysiological recording, neuroanatomical techniques, and functional imaging to examine processing in auditory cortex. Work in the lab examines cortical plasticity in the presence and absence of acoustic input, and following the initiation of auditory processing through the means of cochlear prosthetics. He is the Associate Editor of Hearing Research, and a past chair of the Gordon Research Conference on the Auditory System and the International Conference on Auditory Cortex.
CAA Members free registration
Non CAA members – fee $50.00 CDN
- Archived Webinar: New Advances in Tinnitus Assessment webinar with Philippe Fournier – Aired November 20, 2018
New Advances in Tinnitus Assessment webinar with Philippe Fournier, Ph.D – November 20th, 2018 at 1 pm ET.
CAA Members Watch Now
While masking and residual inhibition (RI) may provide diagnostic and prognostic valuable information, these measures are rarely performed in clinics, as they are not adapted to clinical constraints. This webinar will present a new method for measuring tinnitus masking and residual inhibition by using an acoustic sequence made of pulsed acoustic stimulation of fixed duration and inter-stimulus intervals that may be more suited to clinical constraints. The difference between this new technique and the ‘’classic’’ method will be provided. The results obtained with this new technique from a tinnitus cohort of 64 tinnitus patients will be presented. From the study, it was concluded that, with the new technique, the measurements of tinnitus masking and residual inhibition can be easily, quickly and reliably obtained from a wide variety of patients displaying different hearing loss configurations such as presbyacusis, flat hearing loss and even normal hearing. More so, this approach allows the categorization of tinnitus patients into different sub-groups. The potential of these measures as a prognostic indicator of sound therapy success will be discussed.
Learning Outcomes:
- Understand the concept of tinnitus masking and residual inhibition
- Differentiate the new technique using pulse noise from the classic method to measure tinnitus masking and residual inhibition
- Integrate the new minimum masking level and minimum residual inhibition level technique using pulse-noise in their clinical practice
- Integrate those new results with those of other test in their overall interpretation of the tinnitus condition of a patient
The Speaker: Philippe Fournier, Ph.D., Postdoctoral fellow researcher, M.Sc.S., Audiologist, FAAA
Philippe Fournier is currently a postdoctoral fellow at the Centre national de la recherche scientifique (CNRS), Université d’Aix-Marseille, France. He is also the founder, and past CEO and president of the Quebec Association of Speech-language Pathologists and Audiologists (QASLPA) from 2011-2014. Philippe research has been dedicated to improve diagnostic measures and therapy options for tinnitus and hyperacusis. Philippe also has previous experience as a clinician in a private practice setting in Montreal and as audiology clinical instructor for the audiology clinic of the Université de Montréal.
- Archived Webinar: Motivation, Cognition and Listening Effort with Mary Rudner – Aired June 28, 2018
Motivation, Cognition and Listening Effort 
Speaker: Professor Mary Rudner
CAA Members Watch Now
Hard of hearing people often find that listening is effortful. This makes listening effort an important phenomenon to study. However, there has been a lack of consensus among the research community concerning both the definition of listening effort and how to measure it. The Framework for Understanding Effortful Listening (FUEL, Pichora Fuller et al., 2016) brings together tools and concepts to form a basis for future work on understanding listening effort. It also provides a scientific definition of listening effort: the deliberate allocation of mental resources to overcome obstacles in goal pursuit when carrying out a listening task. Fundamental to the FUEL is Kahneman’s (1973) model of attention and effort, which describes how available cognitive resources are allocated to on-going tasks. This allocation process can also be understood in terms of working memory. The decision to allocate cognitive resources to a listening task often depends on motivation and the pleasure of hearing significant sounds.
In this CAA webinar, I will describe the FUEL and how it can be used as a tool for understanding effortful listening. I will also provide examples of the way in which the FUEL is driving current research.
Learning points:
1. The role of cognition in listening
2. Understanding the Framework for Understanding Effortful Listening (FUEL)
3. Methods of measuring listening effort
Speaker: Mary Rudner, Professor in Disability Research, Linnaeus Centre HEAD, Department of Behavioural Sciences and Learning, Linköping University, Sweden.
Mary Rudner is Professor of Disability Research specializing in Cognitive Hearing Science at Linköping University, Sweden and guest professor at Lund University, Sweden. At Linköping University, she is Deputy Research Manager at the Linnaeus Centre HEAD, for research on HEaring And Deafness, and Director of Studies of the HEAD Graduate School. Her research interest is in the role of cognition in language and memory. Her work is funded by Swedish Research Council, Swedish Foundation for Humanities and Social Sciences, Swedish Council for Health, Working Life and Welfare and she has received career awards from Linköping University. She collaborates nationally and internationally. Recent work has focused on cognitive representation and cross-modal plasticity associated with deafness.
CAA Members Register Now
Non CAA Members – fee $50.00
References
- Kahneman, D. (1973). Attention and Effort. Englewood Cliffs, NJ: Prentice-Hall, Inc.
- Pichora-Fuller, M.K., Kramer, S.E., Eckert, M.A., Edwards, B.B., Hornsby, B.W.Y., Humes, L.E., Lemke, U., Lunner, T., Matthen, M., Mackersie, C.L., Naylor, G., Phillips, N., Richter, M., Rudner, M., Sommers, M.S., Tremblay, K.L. & Wingfield A. (2016). Hearing Impairment and Cognitive Energy: The Framework for Understanding Effortful Listening (FUEL). Ear and Hearing, 37, 5S-27
- Archived Webinar: An Overview of the Development of the Document, “Vestibular Assessment & Management for Canadian Audiologists: A Scoping Review”
An Overview of the Development of the Document, “Vestibular Assessment & Management for Canadian Audiologists: A Scoping Review”
Presented: Tuesday, May 30 at 12 pm EDT to 1:30 pm EDT
CAA Members: Watch the recording now
More Information
- Archived Webinar: Connected Technologies for Improved Access in Global Hearing Care with De Wet Swanepoel – Aired May 22, 2018
Connected Technologies for Improved Access in Global Hearing Care
Speaker: De Wet Swanepoel, Ph.D., University of Pretoria
Watch recording.
Webinar Abstract
Hearing loss is a pervasive chronic disability that affects more than a billion people annually. Unsurprisingly, it is a leading contributor to the global burden of disease. Early access to hearing care is critical for optimal outcomes, but for most of those affected it remains out of reach. Novel solutions, capitalizing on advances in technology and connectivity, demonstrate promise for increasing access and quality of care whilst reducing costs. The penetration and ubiquity of mobile phones, even in developing countries, make connected technologies a powerful potential tool for widespread impact.
This presentation will consider two broad approaches to connected solutions for hearing loss including an end-user consumer model and a point-of-care diagnostic device operated by minimally trained facilitators. The hearZA App – South Africa’s National Hearing Test – was launched on World Hearing Day 3 March 2016 (www.hearZA.co.za). The digits-in-noise test, which is self-administered, is quick and provides a valuable indication of real-life hearing ability – understanding speech-in-noise. The impact of this public hearing health tool will be reviewed along with further developments in accuracy and platform possibilities such as customisable web-apps and freestanding kiosks in community centres.
Targeted community-based hearing tests in contexts such as home visits, schools and primary health care clinics can be facilitated by minimally trained persons using low-cost connected technologies. Our research on Android-based software applications has demonstrated that accurate calibration and real-time noise monitoring is possible on supported devices, which allow for clinically valid pure tone audiometric testing when linked with a calibrated headphone. Connected solutions like these allow new models of service-delivery where minimally trained persons, with support from a cloud-based data management services, can ensure greater penetration, reach and even uptake of hearing health care.
Learning points
- Participants will be able to describe burden of hearing loss globally
- Participants will be gain an understanding on how mHealth solutions can impact hearing care
- Participants will be able to describe new community-based service-delivery models enabled by connected hearing care
Speaker: Prof. De Wet Swanepoel, is professor in the Department of Speech-Language Pathology and Audiology, University of Pretoria with adjunct positions at the University of Western Australia, and is a senior research fellow at the Ear Science Institute Australia. Prof Swanepoel’s research capitalises on the growth in information and communication technologies to explore, develop and evaluate innovative service delivery models and applied solutions to improve access to early development and health services, particularly in ear and hearing care. He has published more than 140 peer-reviewed articles, books and book chapters and has received numerous national and international awards in recognition of his work. Prof Swanepoel serves as president of the International Society of Audiology and as deputy editor-in-chief of the International Journal of Audiology.
De Wet Swanepoel, Ph.D.
- Department of Speech-Language Pathology and Audiology, University of Pretoria, Pretoria, Gauteng, South Africa
- Ear Sciences Centre, School of Surgery, University of Western Australia, Nedlands, Australia
- Ear Science Institute Australia, Subiaco, Australia
- Archived Webinar: Speech Understanding in Complex Environments by Children Who Are Hard of Hearing – Aired Sept 25, 2019
DATE: September 25th, 2019 – 1pm ET
SPEAKER: Dawna Lewis, PhD, Senior Research Associate, Boys Town National Research Hospital
CAA Members Watch Now
(remember to sign in first then select members only links)
ABSTRACT: There is a substantial body of research demonstrating that speech perception by children who are hard of hearing is negatively impacted by poor acoustics. Much of the previous research in this area has been conducted via laboratory studies using speech-recognition tasks with a single talker and presentation via earphones and/or from a loudspeaker located directly in front of the listener. Real-world speech understanding, however, is affected by interdependent factors including characteristics of the listener, the target speech and background sounds, the acoustic environment, and the message/task. This presentation will address timely issues relative to speech understanding in complex environments, focusing on children who are hard of hearing. We will review relevant research and discuss results in terms of implications for real-world listening and understanding. This discussion will be of interest to clinicians who work with children who are hard of hearing and their families and will provide information that can enhance service provision.
Key Learning Points:
- Have knowledge of the effects of room acoustics on speech understanding.
- Have knowledge of auditory and visual factors that impact speech understanding.
- Have knowledge of the effects of task complexity on speech understanding.
SPEAKER: Dawna Lewis, PhD, Senior Research Associate, Boys Town National Research Hospital
Dawna Lewis, PhD, is a Sr. Research Associate at Boys Town National Research Hospital in Omaha, Nebraska. She has presented and published on topics involving pediatric audiology/amplification and hearing assistance technologies. Dr. Lewis is involved in research addressing issues related to amplification and speech perception in children. Recent work has examined the impact of mild bilateral and unilateral hearing loss on children’s speech understanding in complex environments by manipulating acoustic and visual characteristics of the environments and tasks.


























 DATE: Tuesday, November 24th – 1 PM ET
DATE: Tuesday, November 24th – 1 PM ET